OHSS – this world-leading clinic has the 101

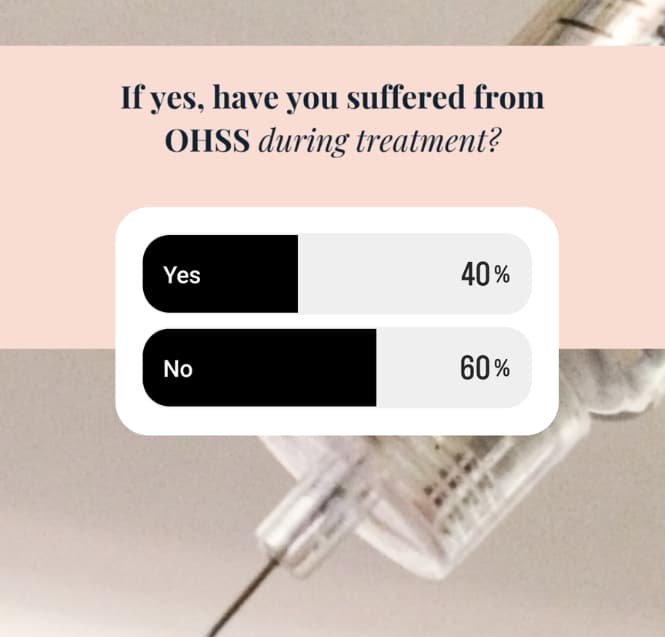
Up to 30 per cent of all IVF cycles are hit by OHSS. That’s the established rate, although this week’s FHH Insta poll (thank you everybody!) reported 40 per cent of respondents had experienced OHSS, during treatment.
Symptoms include abdominal pain, bloating, nausea and enlarged ovaries (keep reading, we’ll cover the full list today), but despite advances in treatment there’s still no cure.
For the team at Laurel Fertility Care – California’s standout fertility clinic group – patient comfort is paramount. So when it comes to OHSS, founder/medical director Dr. Smikle and team are all about prevention first, followed by the most advanced and clinically successful management strategies. Catch his fantastic OHSS expert Q&A with our founder too, while you’re here.
Looking for a patient-first, bespoke approach to your fertility protocol this year? Connect with Laurel Fertility Care and run your history past the exceptional California-based team. From OHSS expertise to PCOS and more, they bring deep, world-leading knowledge to every consultation.
Back to OHSS, here’s everything to know from the experts in patient care, including:
- what it is
- symptoms
- when to see a doctor (we’ll also cover complications)
- successful pregnancy with OHSS
- risk factors
- prevention
- management
FHH & Laurel Fertility Care patient community polls and insights (head to Insta to take part in daily polls)
What is OHSS?
OHSS stands for ovarian hyperstimulation syndrome. It can occur during fertility treatment, usually when you’re taking medication which – alongside stimulating egg development – may cause your ovaries to swell and leak fluid.
OHSS is your body’s response to excess hormone levels. It can be very painful – at best, uncomfortable – and symptoms include abdominal pain, tenderness in the ovaries, nausea, sudden weight gain and extreme bloating.
Occasionally, OHSS can occur when taking medication by mouth – such as clomiphene – but it’s more commonly connected to injectable hormone medication.
Sounds familiar? Frustratingly there’s no cure just yet – in fact, OHSS tends to improve on its own in the majority of mild cases – but severe symptoms may require hospitalization and further treatment. In our Insta poll, around 9 per cent said they’d been admitted to hospital for OHSS.

OHSS symptoms – mild/moderate and severe
Symptoms usually kick in during the week after your ovulation stimulation starts – but it can take longer to start feeling off.
Mild to moderate OHSS symptoms include:
- abdominal pain
- bloating
- nausea and/or vomiting
- diarrhea
- tenderness around your ovaries
Severe OHSS symptoms include:
- rapid weight gain (over 2.2 pounds (1 kg) in 24 hours)
- severe abdominal pain
- decreased urination
- shortness of breath
- tight or enlarged abdomen
Timings, complications & when to see a doctor
Mild OHSS symptoms will usually resolve after about a week. More severe OHSS symptoms can last weeks, however, particularly if you do get pregnant.
But when should you see a doctor? Laurel Fertility Care medical director, Dr Smikle, says,
‘For our team, prevention is priority. We do everything we can to manage risk factors and prevent OHSS symptoms for our patients. But if OHSS is part of the picture, we’re here to help – and knowing your symptoms early on can help us provide effective treatment. Our dedicated team monitor all patients to prevent and catch any reaction you may have to your fertility meds.
If you’re experiencing severe abdominal pain, enlarged abdomen, pain in your legs or shortness of breath, don’t hesitate – call your doctor.’
Complications
While rare, OHSS complications can be life-threatening. They include:
- blood clots
- fluid collection in abdomen and chest
- electrolyte imbalances
- kidney failure
- ovarian torsion (twisting an ovary)
- rupture of a cyst in your ovary, leading to serious bleeding
- breathing problems
- pregnancy loss
Successful pregnancy with OHSS
In the majority of cases, Laurel Fertility Care are able to help patients continue treatment, despite OHSS. And you can absolutely still get pregnant with OHSS – your symptoms may just get a little worse.
Whichever clinic you’re with, you should be monitored closely (just in case). If you’re at-risk of developing severe OHSS symptoms, your specialist may recommend stopping treatment. OHSS complications can be very serious – as we’ve covered – and while it can be very distressing to cancel treatment, we’ll always put your health first and pick treatment up once your OHSS is under control.
25 per cent in this week’s Insta poll said your clinic or team had failed to provide adequate support for your OHSS symptoms and management. So there’s definitely room for improvement – touch base with Laurel Fertility Care if you’re looking to change things up with experienced OHSS support.

Risk factors
OHSS causes and risk factors can be difficult to pin down. We think, however, that these factors may increase its likelihood:
- PCOS (polycystic ovary syndrome)
- having a large number of follicles
- being under age 35
- low body weight
- excessive estradiol (estrogen) levels, before your HCG trigger shot
- having an OHSS history
OHSS is almost always a result of fertility treatment, but in rare cases it can occur spontaneously.
Prevention
Again, prevention is key. To drive down the risk of developing OHSS, we might look at:
- moderating or reducing your meds dosage, while monitoring the ovary’s growth and egg production
- monitoring follicles, looking for fast growth which can lead to them not developing properly (atresia)
- using a medication called Lupron to trigger egg maturation
- restarting Lupron, after egg retrieval
- adding Cabergoline (an oral medication) to help suppress suspected causes of OHSS
Our (amazing) community’s tips and tricks, to manage OHSS
The very best people to ask, when managing a condition like OHSS, are the ones who’ve been through it. We put your FAQs to the FHH Insta community, and here are their top tips for handling OHSS, based on personal experience:
- get lots of rest
- stay hydrated
- focus on a protein-rich diet
- keep an eye on electrolyte imbalance (coconut water is an excellent natural source of electrolytes)
- if you do fancy exercise, go for gentle walking until OHSS eases off
There might not be a cure (yet!) but with careful monitoring and the right team behind you, OHSS can be managed very effectively.

Whether it’s OHSS after egg retrieval or stimulation, PCOS support or the latest protocols for achieving successful pregnancy with OHSS, Laurel Fertility Care are prepped to support you. Connect today to chat through any questions you have.


