No sperm in the sample? Obstructive vs non-obstructive azoospermia, misdiagnosis & new-gen treatment

Hearing that a semen analysis showed zero sperm can completely stop you in your tracks.
This is what happened almost 10 years ago when TRB Founder Eloise Edington and her husband got his results back. For them, questions immediately began to spiral quickly: Can azoospermia be misdiagnosed? How do we know if it’s obstructive vs non obstructive? Does this always mean surgery?
Back then, clear, grounded answers weren’t easy to come by. Information felt fragmented, and knowing what applied to their situation was far from easy.
Fast forward to today, and those gaps in understanding are exactly what TRB exists to help close. For this, we were lucky enough to sit down with one of the most experienced names in the field.
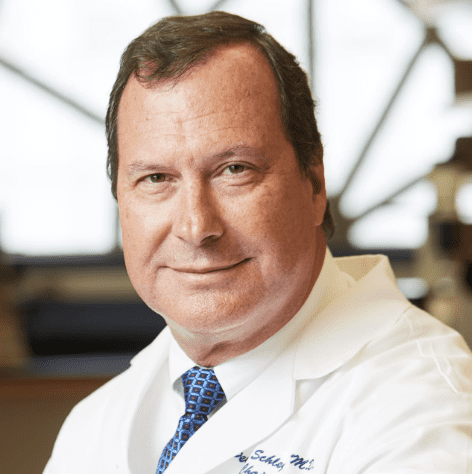
Based in New York, Dr. Peter Schlegel is a world leader in men’s fertility and healthy living.
We nabbed him for a chat to break down some of the most searched questions in the US today, including obstructive vs non obstructive azoospermia, how they’re diagnosed currently and what’s changing right now in the world of treatments and retrievals.
What is azoospermia?
In simple terms, azoospermia is diagnosed when no sperm are seen in a semen sample after proper analysis.
“Azoospermia is a condition where no sperm are present in the ejaculate that can occur because sperm production is very, very low, so low that no sperm survive the trip out of the body. There can also be normal production of sperm, with a blockage preventing sperm from coming out,” Dr. Schlegel explains.
Studies tell us that it affects around 1% of men overall, and up to 10–15% of men with infertility.
Obstructive vs non obstructive azoospermia
Obstructive
“Obstructive azoospermia is a condition where there is completely normal sperm production, so the ability to get sperm and to use them, especially with in vitro fertilization, is excellent,” explains Dr. Schlegel.
Here, sperm are being made but can’t reach the ejaculate due to a blockage. This could be from missing ducts, prior infection, or surgery. Azoospermia surgery is often very effective in these cases.
Non-obstructive
“Non-obstructive azoospermia is where there’s very, very low sperm production overall, and it’s a much more difficult condition to treat because only very rare sperm are typically found,” says Dr. Schlegel.
This form relates to impaired sperm production inside the testicle itself. It’s more complex, but not without options either.
Causes of non obstructive azoospermia
- Genetic factors – Klinefelter syndrome, Y chromosome variations
- Hormonal issues
- Testicular damage – via infections, trauma, radiation, chemo, varicoceles
- History of undescended testes – cryptorchidism
- Environmental toxins and lifestyle factors
“Men with no sperm in the ejaculate because of low production often are born with that condition, or it may be caused by a very severe insult like chemotherapy that’s given for a cancer or radiation therapy.” says Dr. Schlegel.
Causes of obstructive azoospermia
- Congenital causes
- Acquired causes – Infections, trauma, surgical complications
“In other cases, men may have a blockage that prevents sperm from coming out either because they were born with an area of the reproductive system that’s missing. Essentially, the ducts or pathway for sperm didn’t develop, or because they have an infection or otherwise acquire a blockage in their, in their tract,” says Dr. Schlegel.
Can azoospermia be misdiagnosed?
“Yes,” says Dr. Schlegel, and lab technique is often the reason.
“Azoospermia… is very dependent on how the laboratory analyzes those specimens… It is typical in a standard analysis to possibly miss very limited numbers of sperm with a standard evaluation.”
A note on extended sperm search
“So an extended sperm search is actually a more detailed analysis of the fluid that makes up semen to search for very rare sperm,” Dr. Schlegel explains.
“You can miss sperm with a standard semen analysis… An extended search looks at drop after drop after drop to find even very rare sperm in the ejaculate.”
This matters, because finding even a small number of sperm can change the treatment pathway.
Is it possible for azoospermia to resolve on its own?
In a word, no.
“Most men with azoospermia… will fairly consistently have very, very low numbers of sperm or zero sperm,” says Dr. Schlegel.
“But occasionally they will go from zero sperm to enough sperm in the ejaculate that you can actually use them for IVF… It’s unusual for azoospermia to revert back to completely normal sperm production.”
This is why repeat testing can be worthwhile.
Azoospermia surgery options
When sperm aren’t found in the ejaculate, surgical sperm retrieval is often the next step. Here are the three main azoospermia surgery options used today:
- PESA or MESA (epididymal aspiration) – Typically used in cases of obstructive azoospermia, where sperm production is normal but blocked from reaching the ejaculate. PESA is done with a needle. MESA involves a minor surgery and is somewhat more successful.
- TESE (testicular biopsy) – This involves taking small biopsies directly from the testicle to look for sperm. This approach can be used for both obstructive and non-obstructive azoospermia.
- Micro-TESE (microscopic testicular extraction) – The most advanced surgical option and is most often used for non-obstructive azoospermia, where sperm production is extremely limited
What is the difference between TESE and micro-TESE?
“The difference between TESE and micro-TESE is just a series of small biopsies, samples taken of the testicle that are done randomly.
Micro-TESE is a search with an operating microscope that allows you to identify the single smallest, best areas of the testicle, so very little tissue is removed and you have the best chance of finding areas of sperm production.” says Dr. Schlegel.
This precision is why micro-TESE is often used for non-obstructive azoospermia.
Are there any new treatments for azoospermia in 2026?
“There are several areas where people are doing research to improve treatment of men with azoospermia.” says Dr. Schlegel.
- Both AI-based and extended sperm searches – aiming to improve detection of very rare sperm in the ejaculate
- Medications like isotretinoin – an experimental vitamin-A acting agent that may help to improve sperm production in some men
Progress is steady, practical, and focused on finding sperm where they were previously missed.
Want more advice? Schedule a consultation with Dr. Schlegel today to discuss your specific concerns and explore personalized medical solutions.
With his extensive knowledge and dedication, Dr. Schlegel is helping men across New York City and beyond achieve optimal well-being and regain control over their lives.
Watch our social video interview with Dr. Schlegel on male infertility for more of a flavor of how deep his knowledge and expertise goes.
Liked this feature? Read this next: Can you use the same sperm donor twice? Family limits and donor reserve options explained by a leading international sperm bank
View this post on Instagram